Who released a report on ‘Global Tobacco Pandemic Epidemic, 2023: Protect people from tobacco smoke’. The report tracks the progress made by countries in tobacco control since 2008 and, marks 15 years since MPOWER measures were introduced. Read here to learn more about MPOWER and Indian efforts for tobacco control.
With over 8 million tobacco-related deaths a year, tobacco use continues to be one of the biggest public health threats and tobacco control remains a global health priority. This is the ninth WHO report on the global tobacco epidemic and the fifteenth year since MPOWER was introduced as a technical package designed to help countries implement the demand-reduction measures of the WHO Framework Convention on Tobacco Control. This report shows that, in 2022, more than 5.6 billion people, 71% of the world’s population were covered by at least one MPOWER measure implemented at the highest level.
Global Tobacco Epidemic
The global tobacco epidemic refers to the widespread and growing public health issue caused by the use of tobacco products.
- Tobacco use is one of the leading preventable causes of death worldwide and poses significant health risks to both users and non-users exposed to secondhand smoke.
- The epidemic is driven by the consumption and addiction to tobacco products, primarily cigarettes, which contain nicotine and other harmful substances.
The WHO Framework Convention on Tobacco Control (WHO FCTC) and its guidelines provide the foundation for countries to implement and manage tobacco control. To help make this a reality, WHO introduced the MPOWER measures.
- Monitoring tobacco use and prevention policies
- Protecting people from tobacco smoke
- Offering help to quit tobacco use
- Warning about the dangers of tobacco
- Enforcing band on tobacco advertising, promotion, and sponsorship
- Raising taxes on tobacco
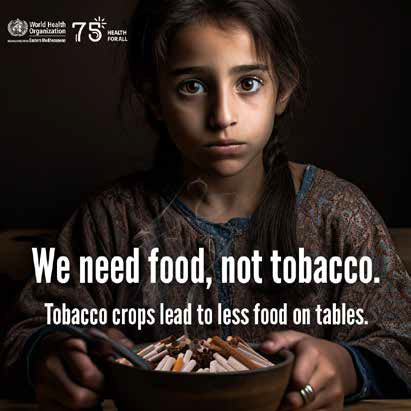
Protecting people fro m tobacco smoke – the “P” of the MPOWER measures – is the focus of this ninth WHO report on the global tobacco epidemic and is a crucial component of the MPOWER package.
 Key highlights of the report are:
Key highlights of the report are:
- In 2022, the number of countries implementing at least one MPOWER measure has increased to 151.
- Only 4 counties (Brazil, Turkiye, Netherlands, and Mauritius) have implemented all measures.
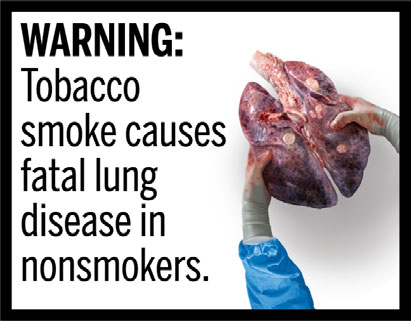
- Tobacco kills more than 8 million people each year, including 1.3 million non-smokers who are exposed to SHS (Second-hand smoking).
- India is ranked among the highest achievers in tobacco dependence.
Facts related to the global tobacco epidemic
- Tobacco use is linked to a wide range of health problems, including various types of cancer (e.g., lung, throat, mouth, esophageal), cardiovascular diseases, respiratory diseases, and reproductive disorders. Smoking is responsible for millions of premature deaths each year.
- Nicotine, present in tobacco products, is highly addictive, making it challenging for users to quit. The addictive nature of nicotine contributes to the persistence of tobacco use despite known health risks.
Non-smokers exposed to secondhand smoke are also at risk of adverse health effects, including respiratory illnesses, cardiovascular diseases, and lung cancer. - The tobacco industry often targets young people with aggressive marketing strategies and appealing product designs. As a result, many individuals start using tobacco products at a young age, leading to addiction and long-term health consequences.
- The tobacco epidemic has significant economic implications due to the high healthcare costs for treating tobacco-related illnesses and lost productivity from illness and premature death.
The tobacco epidemic is a global health challenge affecting developed and developing countries. - Low- and middle-income countries are particularly vulnerable due to the increasing prevalence of tobacco use and limited resources for healthcare.
- The tobacco industry’s marketing and lobbying efforts have been a significant obstacle to effective tobacco control measures. They have also sought to undermine tobacco control policies and regulations that aim to reduce tobacco use.
Tobacco control efforts
Various countries and international organizations have implemented tobacco control measures to combat the epidemic.
- These measures include tobacco taxes, smoke-free policies, graphic health warnings on tobacco packaging, public awareness campaigns, and support for smoking cessation programs.
The WHO Framework Convention on Tobacco Control is an international treaty that aims to reduce the demand for tobacco products, control tobacco advertising, protect people from second-hand smoke, and regulate tobacco product packaging.
India
 Tobacco control in India is a critical public health priority due to the significant health and economic burden caused by tobacco use. The Indian government has taken several measures to curb tobacco consumption and reduce its harmful effects on the population. Some of the key tobacco control initiatives in India include:
Tobacco control in India is a critical public health priority due to the significant health and economic burden caused by tobacco use. The Indian government has taken several measures to curb tobacco consumption and reduce its harmful effects on the population. Some of the key tobacco control initiatives in India include:
- Cigarettes and Other Tobacco Products Act (COTPA): COTPA is a comprehensive law enacted in 2003 to regulate the production, sale, distribution, and advertisement of tobacco products in India.
- It prohibits smoking in public places, selling tobacco products to minors, and using tobacco products near educational institutions.
- COTPA mandates smoke-free policies in public places, including educational institutions, healthcare facilities, offices, and public transport. Smoking is also banned in trains and airplanes.
- Health Warnings on Tobacco Packaging: India was among the first countries to implement large, graphic health warnings covering 85% of the principal display area on tobacco product packaging. These warnings illustrate the adverse health effects of tobacco use and serve as a deterrent.
- National Tobacco Control Program (NTCP): The NTCP was launched in 2007 to support the implementation of tobacco control measures at the national and state levels. It focuses on public awareness campaigns, monitoring tobacco use, and facilitating tobacco cessation services.
- Tobacco Taxation: The Indian government periodically increases taxes on tobacco products to make them less affordable and deter consumption. Higher taxes also generate revenue that can be invested in public health initiatives.
- Ban on Advertisement and Sponsorship: India prohibits direct and indirect advertising of tobacco products. It also bans tobacco companies from sponsoring events, sports, or cultural activities.
- Prohibition of Electronic Cigarettes Act, 2019: In 2019, the government issued an ordinance to ban e-cigarettes and other electronic nicotine delivery systems (ENDS) to prevent their potential harm to public health, especially among youth.
- National Health Policy 2017: The national health policy targets to reduce tobacco use by 30% by 2025.
- Tobacco Cessation Services: The government promotes tobacco cessation through various programs and initiatives. It provides training to healthcare professionals to offer counselling and treatment for tobacco dependence.
- Surveillance and Monitoring: India conducts national and subnational surveys to monitor tobacco use prevalence, compliance with tobacco control laws, and the impact of tobacco control interventions.
India is a party to WHO Framework Convention on Tobacco Control. Tobacco control in India is a dynamic process, and the government, along with civil society organizations and public health stakeholders, continues to work towards reducing tobacco use and its associated health consequences.
What do experts say?
One of the biggest steps in the works is implementing warnings on OTT platform content when actors are seen using tobacco products. “This would make India the first country in the world to do so. And, it is needed. Movie theatres already display such warnings but they are missing when it comes to OTT platforms. During the pandemic, there was a huge increase in the number of people subscribing to OTT platforms. This content is also readily available to children which means the warnings also have to reach them. The initial warnings on movies were brought in because children and adolescents were seeing their icons smoking on screen and taking it up,” said Binoy Mathew, an expert in tobacco regulation from the Voluntary Health Association of India.
He said that India already has a comprehensive law on tobacco control, but some amendments are needed in the 20-year-old law. “There is a need for the law to ban the loose sale of cigarettes. What we see is that many people, especially college students, buy one or two cigarettes instead of the whole pack which might cost R 350-400. This means they are not exposed to the health warning and quit-line at all.”
He felt there was also a need to increase fines for smoking in public places. “Right now, the fine is just Rs 200. That does not deter people anymore.” He even argued for completely doing away with designated smoking areas with restaurants even serving food and drinks in such areas. “Besides, we still see people selling packs of cigarettes from neighbouring countries that do not carry the 85 per cent health warning.”
ABOUT TEAM VHAI
Voluntary Health Association of India (VHAI) is a national public health organization dedicated to making health and development a reality for people of India. It is the largest network of non-governmental health organizations in the world. Bhavna Mukhopadhyay is the Chief Executive of VHAI.